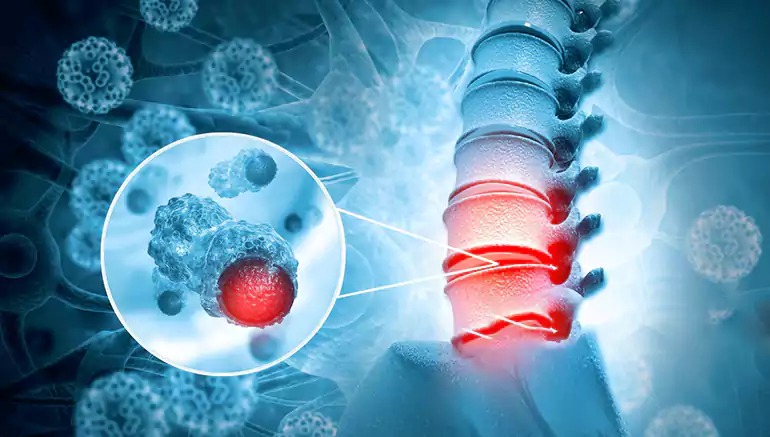
Spinal infections—including vertebral osteomyelitis, discitis, spinal epidural abscess, and Pott’s disease (spinal tuberculosis)—are serious conditions commonly caused by bacteria (e.g., Staphylococcus aureus, Gram-negatives), mycobacteria, or fungi. They can result in severe back pain, fever, neurological deficits, and spinal instability.
Clinical Red Flags: persistent back pain, fever, elevated ESR/CRP, neurological deficits, immunocompromise, or recent surgery or systemic infection.
Imaging: Contrast-enhanced MRI is the gold standard—detects infection within 3–5 days of onset, including epidural or paraspinal involvement. CT and X-ray assess bone destruction. Bone changes on plain films may take weeks.
Microbiological Confirmation: Two sets of blood cultures and CT-guided biopsy (disc and bone) are essential before antibiotics, except in emergencies.
Antimicrobial Therapy:
Empirical IV broad-spectrum antibiotics covering S. aureus (including MRSA), E. coli, and anaerobes—until culture results are available. Common regimens: vancomycin + third-/fourth‑generation cephalosporin or fluoroquinolone.
Duration: IV for ~4–6 weeks, transitioning to oral therapy; total course often 6–12 weeks. For tuberculosis, anti-TB treatment extends to 10–24 months.
Monitor: CRP reduction of ≈50% per week suggests good response; normalization of inflammatory markers and symptoms is needed before stopping.
Supportive Measures:
Initial bed rest (1–2 weeks), followed by ambulation with a brace. Brace type depends on location (neck collar, thoracolumbar brace). Avoid prolonged immobilization in elderly.
Physical therapy initiated once acute infection is controlled to restore mobility and strength. Conservative treatment succeeds in about 90% of stable cases.
Surgery is indicated in cases of:
Neurological deficits or cord compression (e.g., epidural abscess)
Progressive vertebral destruction and instability
Failure of medical therapy (persistent infection or sepsis)
Need for tissue sampling when biopsies are non-diagnostic
Presence of deformity such as kyphosis from Pott’s disease
Surgical Objectives:
Debride infected tissue, drain abscesses, decompress neural elements
Restore stability via instrumentation or fusion
Correct alignment—especially in tuberculosis or destructive bacterial infections
Pott’s Disease (Spinal Tuberculosis):
Common in India, may lead to vertebral collapse, kyphosis, cold abscesses, or neurological compromise. Diagnosis via MRI/biopsy and AFB culture; treated with multi‑drug anti-TB therapy and surgery when indicated. Fungal & Atypical Infections:
Rare but possible in immunocompromised patients (e.g. NTM, Candida, Aspergillus). High suspicion and repeat biopsy may be needed. Therapy is prolonged and tailored based on species.
A. Thorough Evaluation
Integrates detailed history, laboratory workup (ESR, CRP, cultures), high-resolution imaging (MRI ± CT), and biopsy-based histopathology with spinal infection scoring.
B. Personalized Treatment Strategy
Stable, neurologically intact cases → Conservative approach with antibiotics, bracing, early rehabilitation.
Neurological compromise or instability → Early surgical decompression, debridement, and stabilization, followed by culture-directed antimicrobial therapy.
C. Integrated Support
Coordinated care with infectious disease specialists, radiologists, physiotherapists, and rehabilitation teams ensures optimal patient outcome.
D. Monitoring & Rehabilitation
Regular monitoring of inflammatory markers and clinical signs; follow‑up imaging as needed (MRI/CT). Physical therapy tailored to regain function and prevent recurrence.